Signed in as:
filler@godaddy.com
Signed in as:
filler@godaddy.com
Minimally invasive gynaecology, approaching gynaecological surgery laparoscopically (using key hole surgery), vaginally or hysteroscopically has advantages of improved cosmetic outcome, reduced pain and shorter recovery. Advances in surgical technology have enabled most gynaecological surgery to be performed using the minimally invasive gynaecology approach.
Acute gynaecological problems can arise without warning. Conditions like miscarriage, ectopic pregnancy, pelvic inflammatory disease and ovarian cyst accidents are physically and emotionally draining and need a timely response. As the Clinical Lead of the Acute Gynaecology Unit at Royal Women's Hospital, Dr Stephen Lee is the steady hand you need. If you have an acute gynaecological condition, Dr Lee will see you within 24 hours.
Dr Stephen Lee can help with gynaecological problems such as endometriosis and chronic pelvic pain, heavy menstrual bleeding and fibroids, ovarian cysts, vaginal discharge, menopause in women with a history of cancer, uterovaginal prolapse and urinary incontinence, contraception in women with medical disorders, long term contraception, Pap smear abnormalities and sexual dysfunction.

Bartholin cysts and abscesses are some of the most common gynaecological problems, accounting for 2% of all gynaecological presentations to the hospital. The traditional treatment is marsupialisation, which requires a general anaesthetic and is associated with significant post-operative pain. Thanks to surgical advances, these can now be effectively treated using only local anaesthetics with the insertion of a Word catheter.

An ectopic pregnancy is one that has implanted outside the uterine cavity and affects ~2% of all pregnancies. The most common site for an ectopic pregnancy is in the fallopian tube and if surgical management is warranted, most gynaecologists remove the fallopian tube involved. However, in many cases minimally invasive, fallopian tube-preserving surgery in the form of laparoscopic salpingotomy is feasible.

This is a rare pregnancy that has implanted at the site of a previous Caesarean section scar. This is an extremely high-risk pregnancy that in very select cases are allowed to continue and sometimes result in a live birth. In most cases, treatment with intra-sac and systemic methotrexate is recommended. However, due to the prolonged admission associated with methotrexate treatment, surgical management by an expert gynaecologist should be considered.
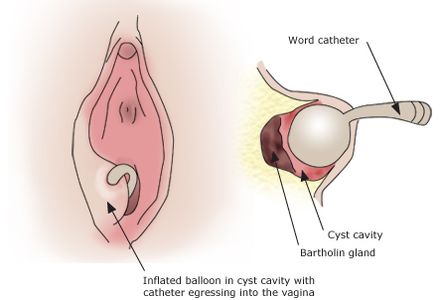
Bartholin cysts and abscesses, which are traditionally treated by marsupialisation under general anaesthesia, can now be effectively treated using only local anaesthetics with the insertion of a Word catheter.
According to the WoMan-Trial published by Dutch gynaecologist Dr Kroese in the British Journal of Obstetrics and Gynaecology in 2016, compared to marsupialisation, insertion of a Word catheter for the treatment of Bartholin cysts and abscesses:
1. Does not require a general anaesthetics and therefore does not require pre-anaesthetic fasting or a prolonged wait to be operated on;
2. Is just as effective with similarly low rates of recurrence;
3. Is associated with less post-procedural pain and therefore patients required less pain relief.
The findings were so overwhelmingly positive, Dr Stephen Lee introduced the treatment modality to the Royal Women's Hospital to successful outcomes and positive patient feedback.

Determining the best treatment for a Caesarean scar pregnancy is a complicated process. One of the predictors for the success rate of medical management with methotrexate is a scoring system devised by Dr Dior's team and published in the Journal of Minimally Invasive Gynaecology in 2019. This scoring system takes into account the pregnancy's gestational age, beta-HCG levels, gestational sac size and the absence or presence of abdominal pain.
In many cases, treatment with intra-sac and systemic methotrexate is recommended. However, due to the prolonged admission associated with methotrexate treatment, surgical management by an expert gynaecologist should be considered. Particularly if the Caesarean scar pregnancy is classified as type 1, which means the gestational sac is developing towards the endometrial cavity, surgical management can sometimes be a straightforward suction curettage. With a type 2 Caesarean scar pregnancy on the other hand (see picture above), laparoscopic removal of the Caesarean scar pregnancy by an experienced set of hands is required. One advantage of the laparoscopic approach is that the Caesarean scar defect can be excised and repairs at the same time.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.